While Joshua James Sánchez Antillón was hospitalized, seriously ill due to COVID-19, his father, Luis Ángel “Wichy” Sánchez Soler, got a bill for $65,000. It did not even itemize the services the hospital was providing.
The invoice issued by HIMA San Pablo Caguas hospital stated that, if signed, he would have 15 days to pay the amount. Wichy Sánchez Soler, who at that time was mourning his father’s death, also due to COVID-19, decided not to sign because he didn’t know what they were charging him for, or how he was going to be able to pay. At that point, the hospital did not offer advice or payment options.
At the end, at just 29 years old, Sánchez Antillón died of COVID-10 and the costs of his treatment exceeded $100,000. His case, the hardships he went through to try to get a proper evaluation, diagnosis and treatment, and the fatal outcome of not receiving prompt medical attention, are the result of the problems that Puerto Rico’s fragmented, and inefficient health system has dragged on for more than two decades.
Sánchez Antillón did not have health insurance because he did not qualify for the government’s health plan for low income citizens, but neither had enough money to pay for a private one, his father explained.
Before falling ill his son had expressed concern about not having health insurance. In fact, not having it could have been the reason for not being tested for COVID-19 and lacking other analyses until the third time he visited a hospital, already decompensated by the disease, Sánchez Soler said.
The young man went to Metro Pavía hospital in Cupey for the first time on March 17, after having been examined by a doctor at Bella International, where he worked as a mechanic. He had not traveled or been in contact with any COVID-19 cases.
Before even evaluating him, they told him he had an outstanding debt from a prior visit. There, they diagnosed him with conjunctivitis and sent him home. He was not tested for COVID-19, despite the fact that since March 4 the American Academy of Ophthalmology had already alerted that conjunctivitis was one of the possible symptoms of the coronavirus. He took several photos of his face in which his eyes were completely red and swollen. His father still keeps the photos as evidence that it did not appear to be typical conjunctivitis, but something much more serious.
His health continued to deteriorate, so he went to the HIMA hospital in Caguas four days later. There, they didn’t do a chest X-Ray or test him for COVID-19, his father said. He went back home and four days later, Sánchez Soler had to take him back to the same hospital because he was very ill. That time, they tested him for COVID-19 and did the chest X-Ray, discovering that he had double pneumonia.
“Nobody could say if he was going to die anyway, but he could have had a greater chance to live if he had been treated in time,” said Sánchez Soler, who thinks that his son was treated differently in the hospitals he visited because he didn’t have health insurance.
The father did everything in his power to help his son. He used his savings and asked family members for help to pay for a medication that cost $12,000 per dose for just two days.
He also did what he could to try to get his son the government’s health plan while he was hospitalized. The first time he filed the application online, he was rejected because his monthly income was around $1,380, when the maximum allowed to get this insurance is $800 a month. The second time he tried, he never got an answer.
Sánchez Antillón was hospitalized for 22 days, until he died on April 15, leaving behind a five-year-old daughter. His father was able to connect with the Medicaid Office through the Centro de Apoyo Mutuo at Caguas after his death. He was accepted retroactively and his father was able to pay $95,287 in medical bills for the hospitalization and an emergency room visit.

Hospitalization bill Joshua James Sánchez.
He was also able to cover other expenses thanks to the help of the Genentech Foundation and through a GoFundMe account that was opened while the young man was still hospitalized.
The Puerto Rico Department of Health (PRDOH) began the contact tracing process for the Sánchez Antillón family on April 1, after the young man’s hospitalization on March 25. The process ended on April 16, a day after his death. Meanwhile, his grandfather Pedro Sánchez Ramos fell ill and also died. Sánchez Soler assured that, despite having lost two direct members of his family to COVID-19, he was tested only when he requested it.
“How is it that I take two people with COVID-19 to the hospital, and they don’t test me?”, he questioned.
COVID-19 exposes cracks in health system
Puerto Rico’s deteriorated and fragmented health system represents a risk to the life and health of Puerto Ricans. This has been proven in recent years during emergencies related to Hurricane María in 2017, the early-2020 earthquakes and now with the COVID-19 pandemic.
The few diagnostic tests carried out, poor contact tracing, mismanagement of tests and infection data, and the lack of a plan to provide services to the uninsured population in the midst of the pandemic, are just some of the situations that have put residents in danger, Puerto Rico’s Center for Investigative Journalism (CPI, in Spanish) has found.
“The only thing the coronavirus has done is the same that (Hurricane) María did: It has exposed the fragmentation of the health system that is unable to run as a single, integrated system, with a comprehensive response, when needed. It cannot do it,” infectologist Lemuel Martínez, president of the Puerto Rico Society of Infectious Diseases, told the CPI.
Dr. Martínez maintained that Puerto Rico’s health system, as in countries where services are mostly private , is not prepared to respond to this type of public health emergency because it depends on private hospitals that have limited resources and budgets, and depend on unilateral reimbursements from health insurance companies.
In other industries, such as the food and fuel businesses, there are regulated rates and price control during emergencies, such as in hurricanes. However, in the health industry, this is not the case, Martínez pointed out, noting that COVID-19’s lessons should provoke changes in regulations and public policy that lead to a better response.
He added that it is important to see the system’s problems and its response to COVID-19 from its core. For example, he said that since the government’s health insurance changed to Plan Vital in 2018, giving way to all health insurance companies to participate in all of Puerto Rico’s regions, 66% of infectious disease doctors were excluded, preventing them from caring for its 1.3 million patients.
The remedy came in May, when COVID-19 had already killed 136 people, and it was a partial one, because who pays for hospitalized patients is still uncertain, the doctor confirmed.
“This is why the managed care model is so dangerous,” Martínez warned , referring to the government’s health plan model in which health insurance companies contract provider networks, but those doctors do not necessarily provide services in hospitals where the patient goes for treatment.
He argued that there are some serious problems with the plan’s model in which the government and its Health Insurance Services Administration (ASES in Spanish) have focused on negotiations with health insurance companies and cost control and have disconnected themselves from the practical reality of the services that patients receive.
Since the virus-related emergency began, through June 30, some 194,000 molecular tests had been done in Puerto Rico, which yielded 2,627 positive results. But the PRDOH has not specified how many were single tests, which prevents knowing the reality of contagion on the island. Up until May, Puerto Rico faced a shortage of tests, the situation was temporarily resolved, but since July 14th laboratories and the PRDOH reported that they were experiencing shortages again.
The lack of available tests responds in part to corruption schemes that benefited those close to the New Progressive Party, that have led to the launch of local and federal investigations. It also responds to the lack of proactivity and trained personnel in the PRDOH, an agency undermined by decades of breakdowns and political appointees not trained in public health.
“The main problem with this emergency is that our Health Department has been decimated for years. That’s why an entire health structure for the population was dismantled, which included tracking and surveillance units,” said Rafael Torregrosa, president of the Puerto Rico Health System Multisectoral Council, created by law in 2015, to analyze the existing models and make recommendations to the Governor and the Legislature.
Faced with this reality, the government, not ready to handle the pandemic, began to improvise, with minimal resources for the programs that are supposed to track and perform epidemiology work on diseases such as Zika, Chikungunya and dengue.

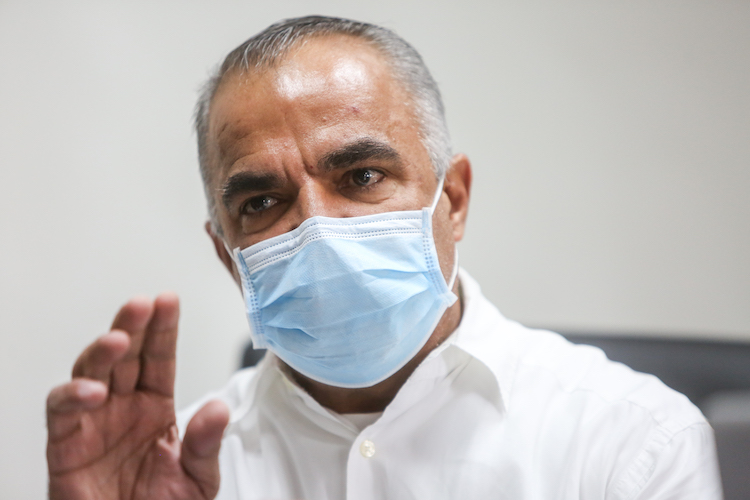
Rafael Rodríguez Mercado
The PRDOH’s most recent stumble came during former Secretary Rafael Rodríguez Mercado’s tenure, who had no experience in administration or public health, and kept on working at his private neurosurgery practice, leaving the agency’s day-to-day operations in the hands of Mabel Cabeza, a political activist with no expertise or experience. Cabeza — a personal friend of the family of Elías Sánchez Sifonte, campaign director of ousted Gov. Ricardo Rosselló Nevares — was in charge of channeling questionable multimillion dollar contracts and recruitments.
Rodríguez Mercado led the disastrous response to the Hurricane María emergency, which took nearly 3,000 lives, according to the official government estimate, and was fired by current Gov. Wanda Vázquez Garced. His successor, Dr. Lorenzo González Feliciano, has acknowledged in several interviews with the CPI that he found a PRDOH in “a precarious situation,” without staff and with multiple mismanagement situations.
Upon arrival, he fired Cabeza, canceled contracts, and ordered investigations into what happened before he joined the agency, including more than $40 million in failed COVID-19 test purchases. The disarray at the PRDOH at all levels and the mismanagement of those purchases are among the main reasons for the government’s slow and poor response to the pandemic.
The current COVID-19 situation in Puerto Rico is that, even though the establishment of a four-month curfew in different stages appeared to have contained the disease, there has been a sharp rebound that started June 22nd and exploded with sustained record hospitalizations the second week of July. And the PRDOH still does not have accurate data on how widespread the contagion is.
“It is obvious that a lot of work was not done from 2012 to 2020 when I got here, that’s when we noticed that the information technology area was weak,” González Feliciano said, to questions about how he compares the current PRDOH with the one he left after his first tenure as Health Secretary.
Lorenzo González Feliciano
In addition to deficiencies in the technical and data systems, he said there were not enough epidemiologists to do contact tracing, nor medical directors in the agency’s seven health regions.
He said he was concerned that there was no capacity to respond to the emergency, because the agency was used to dealing with tracing a few cases of other diseases, so he has been working on recruitment of personnel while simultaneously managing the pandemic.
One of the most important hires, he said, was of Epidemiologist Fabiola Cruz in late May, to establish a tracing program similar to the one she successfully implemented in Villalba, in the central mountains region, at the end of March. Through this program, the agency has already added 69 municipalities to the tracing program, and is assigning them $30 million for the task, he said.
“Along the way, we’ve had to make significant changes within the [health] system to get to where we are, not only regarding the technological infrastructure, but thinkers, computer scientists, and obviously we have made significant changes,” the official said.
He added that there are still important changes to be made, in the regions and in the Planning office, which he hopes will be ready before December.
Although, so far the confirmed deaths of COVID-19 patients in Puerto Rico have been few in comparison with the United States and the world, the total number of deaths in Puerto Rico has increased during the months of the pandemic without any explanation, CPI found. This, contrary to what González Feliciano and the director of the Demographic Registry, Wanda Llovet, said.
The contact tracing system has also been ineffective at the Puerto Rico level due to the lack of staff and the fragmentation of Puerto Rico’s hybrid health system, Epidemiologist Andrés Juliá Beltrán and Infectologist Martínez concurred separately.
Martínez and five other infectologists consulted by the CPI agree that, in line with scientific studies on COVID-19’s behavior, between 80% to 85% of patients who go to the emergency room with symptoms of the disease are not hospitalized but sent back home to recover .
In particular, a study of 72,000 patients in China published by the American Journal of Medicine (JAMA) found that 81% of those infected with the virus who develop the disease show mild symptoms, 14% moderate symptoms, and 5% develop critical symptoms.
In the cases of people who have mild or moderate symptoms who are discharged from Puerto Rico’s emergency rooms, there is no medical professional in charge of doing the molecular test and taking responsibility for following up on the patient, Dr. Martínez told the CPI.
According to best practice guidelines for caring for virus patients, only people with a serious clinical scenario, such as a high amount of oxygen or saturation in the blood, are hospitalized, he said.
“That was one of the things that we called out from the start, because 80% to 85% of patients aren’t going to require hospitalization, and you can’t expect that the hospital that is handling patients (at the ER) will take care of that. There was a disruption because the Department of Health doesn’t have the resources to do it,” Martínez said regarding the tests and follow-up to discharged patients, and the contact tracing.
The situation has forced municipalities to establish their own tracing systems. Both Martinez and Juliá said they have an expectation that contact tracing will finally begin to improve on a larger scale with the new PRDOH’s contact tracing director.
The 330 Health Centers, federally funded health management groups, also began contact tracing after getting an $8.5 million allocation, said Alicia Suárez, director of the Puerto Rico Association of Primary Health (ASPPR, in Spanish). The screening they are doing is a traditional one, through calls, as they have done in the past with other diseases, she explained.
The information has to be shared with the PRDOH, so they could be duplicating efforts, warned Darielys Cordero, director of Special Programs for the ASPPR.
“Talks are underway to see how health centers can be integrated into the efforts that some municipalities are working on, with the idea of avoiding duplicating efforts and maximizing resources, because what we want to avoid is that 10 different organizations are calling the same patient,” Cordero said.
However, despite everything that had not happened, on April 30, the day with the highest number of hospitalizations for COVID-19 at that point since the beginning of the pandemic, with 201 cases, the Governor announced an executive order that would allow the reopening much of the economic sector as of May 4, contrary to the recommendations of the Medical Task Force that she herself appointed to advise her administration on the emergency response strategy. Vázquez Garced buckled under the pressures of her Economic Task Force for the reopening, allowing activity to resume in shopping malls, fast food restaurant dining areas, and beauty salons, which are non-essential nor high-impact areas of the island’s Gross Domestic Product.
On July 14, hospitalizations reached 206 cases, and since the preceding weekend the Medical Task Force’s Epidemiologist, Dr. Juan Carlos Reyes, had been making rounds in the media warning that changes to the reopening policy had to be made. Vázquez Garced did not act, but rather put off making a decision until the end of the week.

Wanda Vázquez Garced
Who pays for the uninsured?
Compounding the problems described is the matter of the uninsured, currently estimated at almost 210,000 people, out of the 3.2 millions island’s population, according to the most recent Census figures. These people, for the most part, do not qualify for the government health insurance plan, but they cannot pay for a private plan either. They are in limbo, since the Department of Health has not created the regulation ordered by the Law to Fight COVID-19, which was signed on April 16 to guarantee that no Puerto Rico resident will pay for COVID-19 testing and treatment. The regulatory framework is supposed to lay out how the medical expenses and testing of the uninsured will be paid for, among other issues.
In its introduction, the law establishes: “to create the Government of Puerto Rico’s public policy regarding the handling of the coronavirus, to provide that all medical care, studies , analysis, diagnosis and treatment of COVID-19, including hospitalization, will be free of charge for all citizens, regardless of whether they have health insurance.”
It also establishes that no health insurance organization, insurer or pharmacy benefit administrator may require a copayment or deductible, referral or pre-authorization in the coverage of virus treatments. Nowhere in the law does it explain how these expenses will be covered.
The regulations for this law, that do not yet exist, must include a list of screenings, tests and medications needed to diagnose and treat COVID-19. Dr. González Feliciano could not pinpoint to the CPI the status of the regulations to implement this law.
Víctor Ramos, president of the College of Surgeons, said health insurance companies are not covering the full cost of COVID-19 testing, despite this law and federal Cares and Families First acts, which also prohibit deductibles to be charged. The doctor said the situation arises from an order issued by the Puerto Rico Insurance Commissioner stating that there must be a clinical reason for health services to be covered.
Ramos said health insurance companies are also paying laboratories less for COVID-19 tests, which has increased the number of laboratories that are not doing them because they cannot shoulder the cost of the uninsured portion.
He added that when a doctor writes up a medical order for a patient to undergo the molecular and serological tests, health insurance companies do not want to cover them both the same day, causing the patient to be exposed during two visits to the laboratory.
Ramos said this situation with health insurance companies is not new, since there are about 150 tests that community laboratories don’t do because it costs them more to do the test than what the companies pay them.
Although the Governor said on Twitter that she ordered the Health Secretary and the Insurance Commissioner to instruct the health insurance companies to assume the cost of the COVID-19 tests, Ramos insisted that the Commissioner did not make any changes to his order.
González Feliciano told the CPI last Tuesday that this matter “was resolved,” but did not specify how medical insurance companies are being forced to cover the full cost of the tests, or who will pay for the uninsured.
Dr. Alexie Lugo Canales, the Patient’s deputy Ombudsman, said that despite the enactment of the Law to Fight COVID-19, he doesn’t know how it will be handled in the case of the uninsured.
“We know there are some primary health centers, the 330s, that are providing free services for those who don’t have health insurance or have financial difficulties. But, what if I want to have (the test) done in a laboratory near my house?”, the official questioned.
More importantly, the 330 Health Centers don’t hospitalize patients, nor do they cover hospitalization costs, which is the most expensive part of treatment. Hospitalizations for COVID-19 can last 20 days or more and studies have estimated that the cost of such a stay can fluctuate between $20,000 and $73,000 in the United States.
Although there is yet no research in Puerto Rico on the average cost of a hospitalization, the federal government has estimated that the cost of a hospital stay for the virus is “at least” 20% more expensive than a regular hospitalization, the President of the Hospitals Association, Jaime Plá, told the CPI.
That said, a hospitalization for COVID-19 in Puerto Rico could cost between $1,440 and $1,920 a day without including other expenses or intensive care, he estimated. The director of the organization that groups the majority of the island’s hospitals stressed that this amount can increase when the patient has other health conditions, requires additional care, or to extend the stay. The estimate also does not contemplate the use of expensive medications or treatments, such as plasma and Resmidivir, he said.
The average COVID-19 hospitalizations in the United States are nine to 13 days, according to the CDC and a study published by the University of California, Berkeley and the Kaiser Permanente health consortium. However, there are patients whose hospitalization has lasted up to 40 days and beyond.
So, the cost of a COVID-19 hospitalization in Puerto Rico, as in the United States, may exceed $100,000, as in the case of Joshua James Sánchez Antillón.
Prior to a hospitalization, or if the severity of the disease does not reach that point, patients will have been given required primary or emergency services. Alicia Suárez, director of the ASPPR, said the 330 Centers receive funds to provide this type of service to the entire population regardless of their status as insured and their ability to pay. However, she pointed out that these services are only at the primary level and that once the patient requires hospitalization, they are referred to other institutions.
Washington-based Puerto Rico’s Resident Commissioner Jenniffer González’s website noted that $1 billion in federal funds was allocated in March to reimburse the costs of tests and medical services for uninsured people that will be channeled through the Fiscal Agency and Financial Advisory Authority (AAFAF, in Spanish), ASES and the Medicaid Office, under the Families First Coronavirus Response Act. But the Secretary of Health said he does not know how these funds will be channeled and which agency has jurisdiction.
“I don’t have the answer,” he told CPI.
Regarding the allocation of funds from the Cares Act, the director of Medicaid in Puerto Rico, Luz E. Cruz Romero, said they are working on what could be a special health insurance plan for the uninsured, but only for expenses related to COVID-19. She explained, initially, the expenses would be paid by the Government of Puerto Rico with funds from the PRDOH, and then the agency would get a refund from the federal government.
Cruz Romero told the CPI that they are still analyzing, together with ASES, how they will provide coverage through the special COVID health insurance plan. Although the money is available, there is no start date yet and Cares funds can be used only until December 31 of this year.
On June 18, the Governor announced during her State of the Commonwealth address that she had extended the coverage of the Plan Vital to 200,000 persons that did not have health insurance. This turned out to be false.
Although the Governor wanted to project that this already happened, a day later, ASES Executive Director Jorge Galva said through a Facebook post that they presented several sustainability proposals for Plan Vital to Congress, including an increase in Puerto Rico’s poverty level to bring it up to 85% of the federal poverty level and be able to expand coverage. At press time, this approval requested in May has not occurred.
Currently the poverty level established in Puerto Rico to be eligible for the Government health insurance plan is an income of up to a maximum of $800 per month. If approved, a person living alone may have an income of about $1,100 per month and be eligible to the new plan.
The Director of Medicaid for Puerto Rico also acknowledged that the Centers for Medicare and Medicaid Services (CMS) had not yet approved the amendment to the State Plan needed to add the 200,000 people to the Plan Vital that Vázquez Garced announced. They also had not gotten funds from the Fiscal Control Board either.
She said they are counting on the amendment’s approval and once passed, it will be retroactive to July 1.
Despite the fact that in December 2018, the Resident Commissioner celebrated the increase in the federal government’s matching for the Medicaid program from 55% to 76%, Puerto Rico is the territory that receives the lowest matching funds, said Japhet Rivera, former Assistant Secretary of Planning, Development and Federal Affairs of the PRDOH. The other territories receive 85% matching, he said.
In Torregrosa’s opinion, the proposal before Congress and the CMS is positive, but transitory, since they are not recurring funds. He explained that the money to support the Puerto Rico Medicaid program must be requested from Congress every two years or when it runs out.
Torregrosa said the Multisectoral Council has insisted that an actuarial analysis be made to find the best way to finance the health system, not only for the medically indigent, but for the entire island’s population.
“It is a political issue to provide a health insurance plan to people, but then they have to go out and look at how to pay for it in subsequent years,” Dr. Ibrahim Pérez, San Juan’s former health director, said about the Governor’s announcement.
“This is the never-ending story. They have been saying that for the last 20 years,” he added about the constant pilgrimage to Congress to seek funds for the government’s health insurance plan. He said it’s not sound administration policy to spend money that is not available.
Dr. Jorge Hess, president of the Puerto Rico Association of IPAs, which groups the primary doctors of 58% of the Plan Vital’s insured, told the CPI that, given the high unemployment rate caused by the economic shutdown as a result of the pandemic, it is expected that at least 150,000 people will apply for this benefit.
As of mid-June, Puerto Rico had the highest rate of insured unemployment (the percentage of people receiving the unemployment benefit in proportion to the workforce) of all U.S. jurisdictions, with 23% and 300,000 people requesting the benefit, according to the U.S. Department of Labor and the Puerto Rico Department of Labor.
Despite high unemployment numbers, the Medicaid Office in Puerto Rico had only received 30,750 applications for Plan Vital, representing 42,679 people, since the emergency began through June 5, according to the director, who acknowledged that she expected a higher number of applicants.
But the truth is that the Medicaid offices have been closed since last March 15, the agency only accepts applications online, and has not oriented the population on how to access the benefit in the current circumstances, nor has it carried out a massive campaign on the issue.
Although the government has already started having employees from certain areas return to their offices, the director indicated that they will continue to work remotely and handle requests virtually. They still do not have a date for when they will open their offices to the public due to a lack of personal protection equipment for the employees, such as acrylic panels for desks and face masks.
An avalanche of new beneficiaries to the Plan Vital would be devastating for the government’s finances, according to former Health Secretary Enrique Vázquez Quintana, and the president of the Multisectoral Council, Torregrosa.
The latter said he does not know how the Medicaid Program will cover a large and permanent increase in its population, since the federal money is only for the emergency, and “that’s not enough.”
Meanwhile, the director of the Puerto Rico Primary Health Association said although they are not yet seeing an increase in the uninsured due to unemployment, she expects an increase in uninsured patients and patients in transition from private health insurance plans to Plan Vital.
The executive assured that they are supporting the Department of Health to ensure that people who come to the 330 Centers apply for the government’s health plan. In the event that a patient does not qualify, they can be treated at the centers paying discounted rates, according to a scale that corresponds to their income level. People below the federal poverty level pay only nominal costs.
Decades of a deteriorating health system
In the 1960s, the government of Puerto Rico had established a comprehensive public health system by levels and ahead of its time, known as the Arbona Model. Decades later, after years of budget deficits and complaints about services, the system underwent a drastic change starting in 1993 when Governor Pedro Rosselló González – father of ousted Governor Rosselló Nevares – introduced a new model, baptized as the Health Reform, the same as the failed initiative by President Bill Clinton. With it, Rosselló González sold most of the public health facilities, replacing government services with contracts with private health insurance companies. He said then that he sought to democratize health services and that all citizens have guaranteed access to the same quality of services, regardless of their economic resources, while at the same time stopping the government’s losses.
“The issue is that one of the (Puerto Rico) Health Reform’s goals was to cover the medically indigent and give them good quality medicine. And now it turns out that it is estimated that there are between 200,00 and 300,00 people in Puerto Rico without health insurance. That did not happen in 1993 under the Arbona Model, where anyone could go to the government and receive care,” said Dr. Pérez.

Joshua James Sánchez Antillón’s death certificate. The young man didn’t have health insurance.
The new health model that Rosselló González implemented, which was based on the concept of capitation — a fixed monthly amount paid per patient to a primary doctor from which hospital and specialist services are subtracted — began to have problems of access for patients, limitation of services by private providers and large annual deficits for the government since its inception.
It also created a fragmented health system that includes public components of the central and municipal governments, and a large private component. In this system, the parties frequently do not communicate with each other, and the government continues to assume the highest costs of tertiary and catastrophic services.
Vázquez Quintana, Health Secretary at the time, and who said that Rosselló González fired him for not agreeing with the creation of the government’s Health Insurance Plan, said in an interview with the CPI that “the (Puerto Rico) Health Reform has problems and had them since 1994 to the present.”
“The problems that the government’s health insurance plan has faced are well known to everybody, and also, that it hasn’t seen significant changes to improve services to Puerto Rico’s medically indigent population. Many people, including health service providers, long to return to the previous health system,” said Vázquez Quintana.
He added that in 2014, when under the Alejandro García Padilla administration the government’s health insurance plan went from one to five private health insurance providers to run the public plan, the system deteriorated even further. Today there are still five companies participating: Triple S, First Medical, Plan de Salud Menonita, MMM and Molina Health, which is on its way out.
“Nobody oversees the health insurance companies,” Vázquez Quintana criticized, while saying that they make a “scandalous” amount of money from their contracts to administer the government’s plan. The CPI asked ASES for the amount that the government’s health insurance companies earn, but as of press time, the agency had not provided the information.
Torregrosa, president of the Multisectoral Council, agreed with Vázquez Quintana that after the Reform was created and implemented “it was the most serious damage done” to the public health system.

The Multisectoral Council that wrote the report ‘The Health System has had enough patches’ in 2016.
“When Rosselló (González) wanted to adopt the model that some states already had, beginning in the 1990s, which was directing health care through for-profit health insurers companies, everything fell apart here,” he said.
“Two things have been running in parallel: one is the financing done through the insurers, and the dismantling of the health system’s leadership or governance. But rest assured that the companies run the show,” he added.
Governance is defined by the World Health Organization (WHO) as “the most complex and critical component of any health system, which implies the general leadership, regulation and supervision of the entire health system — public and private, to protect the public interest.” Governance has three elements: transparency, accountability, and participation.
Torregrosa said that, according to a study, administrative expenses of more than one insurer’s health plan model has increased to 34.2%.
“In other words, the system that we have generates losses due to excess administrative expenses: 34.2 cents for every dollar. From the get-go, under this model, you have lost more than one-third of the money,” he explained.
He said this situation could perhaps be resolved with a single payer system.
Torregrosa said that if there was a time when the health system was being properly managed, it was in 1974, when the island enjoyed a better life expectancy compared to the rest of the world. At the time, he said, there was a properly functioning regionalized system and there was a universal system, since practically all Puerto Ricans were covered.
After that, the situation deteriorated, prior to the establishment of the Reform, due to the “addiction” of participating in federally funded programs.
Dr. Pérez said beneficiaries covered under the Arbona Model have been currently reduced by almost half, but eight times more is spent versus 1993, when Rosselló Gonzálezs reform began. He said the cost that each beneficiary represented to the government was $524 a year, versus the $3,721 per person under the Plan Vital.
Pérez said that the change in the Arbona Model to the Rosselló González reform came about because he adopted the reform that President Bill Clinton wanted to implement, which was ultimately not approved in Congress. It offered Rosselló González $430 million annually to run the government’s plan.
“In other words, Rosselló (González) was taking advantage of the fact that instead of the $40 million in Medicaid funding that he had until then, the Clinton reform was going to give him $400 million annually and that was going to let him finance his reform in Puerto Rico. But since that money never came, then they had to resort to the government’s general fund and during all those years they continued to finance it with the government’s general fund,” he said.
He recalled that in 2010, when ASES was placed in syndication, it was suggested that Puerto Rico’s bankruptcy was caused by the annual shortfall of the Health Reform, which did not have the financing promised by the federal government.
Most of Vázquez Quintana’s successors, including the late Health Secretary, Johnny Rullán, and former Secretaries Rosa Pérez Perdomo and Ana Ríus, were also critical of the new system. However, none made fundamental changes to the model.
It took 15 years for the first in-depth assessment to be done into the change that had such a profound impact on public health and government finances.

Dr. Jorge Sánchez
The first and most sweeping evaluation of Puerto Rico’s health system in modern times was done in 2005 by the Puerto Rico Health System Evaluation Commission, appointed through an Executive Order signed by Governor Aníbal Acevedo Vilá.
The analysis, led by Dr. Jorge Sánchez — former University of Puerto Rico president, a member of the Medical Sciences Campus staff, and member of the political opposition — took 10 months and involved more than 100 professionals from different disciplines, from the public and private sectors.
It concluded with a 318-page document that made important recommendations and whose main verdict was that Puerto Rico should move toward a Universal Health Plan in which there was a minimum basic coverage to which all residents of Puerto Rico were entitled, regardless of their economic capacity.
Sánchez pointed out in an interview with the CPI that when they decided to do the evaluation, the Health Reform established by Rosselló González had been running for 12 years, without any improvements or analysis done.
“The system was incoherent, fragmented, of sketchy quality, expensive, and there was no incentive to keep communities healthy. Health insurance companies had control of the system,” he said.
He recalled that in 1954, under Luis Muñoz Marín administration, Puerto Rico established a regional and tiered health system that was a model for other parts of the world. The plan, later baptized with the name of the Health Secretary who promoted it, Guillermo Arbona, included the construction of the Puerto Rico Medical Center, regional secondary hospitals, and primary centers in the municipalities. Over time, the system deteriorated and became indebted, and in 1993 Rosselló González privatized it and completely changed the service model overnight.
The doctor said that in the beginning, the current system seemed to have great possibilities of success, but it was implemented too quickly, and the power of the health insurance companies was decisive. Added to this was the lack of government resources and harmful CMS guidelines. Some of the Commission’s most pressing recommendations were the need to group and harmonize all government health plans and services under the PRDOH, including the operations of ASES.
It also raised the urgency of solving the serious problems of operational fragmentation and financial instability of the hospitals comprising the main Medical Center, and the redundancy and inefficiency of what he called a “subsystem” of emergency rooms throughout the island that was established on the basis of political considerations rather than medical necessity, and finally, solving the problem of the uninsured — at that time 300,000 — incorporating them into the plan according to their income level.
None of this has happened.
After delivering the 2005 Commission report, only the prevention system was addressed with a transfer of funds from ASES to the PRDOH, and changes to the provision of medicines through private companies were made.
“I don’t think it went beyond that,” Sánchez said.
Former Governor Rosselló González refused to answer questions for this story about the state of the Puerto Rico health system that he designed and implemented.
Despite the studies, the opinion of experts, and the fact that in March he found a PRDOH without resources, Secretary González Feliciano stands by the privatized model, arguing that there were problems with access to medicines under the previous model.
He also told the CPI that “the idea of having a universal plan is a fallacy,” although there are other countries in the world that have it. He maintained that Puerto Rico’s current health model is the same as that of the states.
“We have a system already running that can be improved…,” he said.
Sánchez disagreed. He noted how now COVID-19 is bringing many of the health system’s problems to the forefront and brings out the need for human resources, budget, space, laboratories, and the expertise to attend to a disease that is unknown and that shows new variations on a daily basis. The emergency unveils a PRDOH without resources.
“No one expected the pandemic, and that’s basically the point: you add this to an incompetent system that consumes the resources you have. In addition to that, we’re unable to establish surveillance, monitoring of laboratory tests, and arrangements with hospitals to deal with a new outbreak of COVID-19, which is coming,” he predicted.
He said the mayors who have assumed the responsibility of the State in this situation have been the salvation.
“As of today, we can say that Puerto Rico’s health system is as deficient now as it was in 2005. It’s the government’s duty to ensure the ‘HEALTH’ of the people, therefore a new form of universal health insurance is required for everyone in Puerto Rico,” said Sánchez.
Universal health insurance would also solve the problem of the 200,000 uninsured who, like Joshua James Sánchez Antillón, are unprotected in the face of COVID-19, he concluded.
This story is published in part with the support of the Ravitch Fiscal Reporting Program of the Graduate School of Journalism at New York City University.


